RESEARCH ARTICLE
Hippokratia 2019, 23(2): 58-63
Gkouvas G1, Agathangelidis F 2, Nakas C 3 , David C 4, Sagris D 4, Petsatodis G 2
1424 Military General Hospital, Thessaloniki, 21st Department of Orthopaedics, Aristotle University of Thessaloniki, General Hospital G.Papanikolaou, Thessaloniki, 3Laboratory of Biometry, School of Agriculture, University of Thessaly, Volos, 4Mechanical Engineering Department, School of Engineering, International Hellenic University, Serres, Greece
Abstract
Background: Intramedullary nailing is the “gold standard” treatment modality of diaphyseal fractures of the tibia. However, when the same method is used for extra-articular fractures of the proximal tibia, various problems may occur, like malalignment, loss of reduction, and non-union. The objective of the present biomechanical study was to compare the stability of six tibial nails when these are used for the treatment of unstable, extra-articular, proximal tibial fractures.
Methods: Thirty composite tibia models were divided into six groups, and a corresponding number of nails from six manufacturers (Citieffe, Braun Aesculap, Orthoselect, Orthofix, Stryker, and Depuy Synthes) was implanted in each group. The maximum number of proximal screws was used for each specimen, and a proximal gap osteotomy was performed. Each bone model was then submitted in dynamic, followed by static loading, and the passive construct stiffness was calculated, representing the specimen’s rigidity. Furthermore, for each specimen, the force needed to cause a displacement of more than one millimeter at the fracture site was calculated.
Results: Stiffness values of a solid nail with two proximal screws and a cannulated nail with five screws were significantly higher compared to all other groups. On the other hand, a titanium cannulated nail with three screws showed the lowest rigidity.
Conclusion: Solid nails provide more rigidity compared to cannulated ones, and the maximum number of proximal screws in all possible directions should be used in order to achieve maximum stability. HIPPOKRATIA 2019, 23(2): 58-63.
Keywords: Intramedullary nail, tibia fracture, proximal, screws, biomechanical study
Corresponding author: Filon Agathangelidis, 39A Stratigou Sarafi str., 55132, Kalamaria, Thessaloniki, Greece, tel: +306974072836, e-mail: fagath@gmail.com
Introduction
Intramedullary nailing remains the treatment of choice for unstable tibial shaft fractures due to excellent healing rates, with minimal procedure-related complications1,2. As a result of this gain in popularity, the indications for intramedullary nailing have expanded to more proximal and more distal fracture patterns. Soon after the implementation of intramedullary nailing of proximal and distal tibial fractures, problems such as unacceptable malalignment have surfaced3. This is mainly due to the flared triangular shape of the proximal and distal metaphysis, which prevents cortical contact of the nail. Regarding the distal tibia, it has been shown that it is necessary to achieve an acceptable reduction using meticulous surgical techniques, followed by at least two distal locking screws in order to have the optimal bone-implant interface, which will lead to union4,5.
Treatment of extra-articular proximal tibial fractures with an intramedullary nail remains challenging. Valgus malalignment and anterior angulation of the proximal fragment are common deformities that led some authors to advise against the use of intramedullary nails for the treatment of these fractures6. Several reasons for this issue have been identified, such as the anteriorly directed pull of the extensor mechanism of the knee, the mismatch between the diameter of the nail and the metaphysis at this level, the inappropriate entry point and inability to use at least two proximal locking screws in the short proximal segment7. Various adjustments to the standard intramedullary technique have been proposed, which aim to achieve and maintain an acceptable reduction. These include the use of blocking-poller screws8, a more lateral entry point9, nailing with the knee in an extended position10, suprapatellar nailing11, and modification of the proximal interlocking screws position, number and orientation12.
The aim of the present biomechanical study was to evaluate and compare the properties and behavior of six modern, commercially available intramedullary nails for the treatment of proximal extra-articular tibial fractures.
Materials and methods
Thirty composite bone models of the tibia were used (Model number 3401, 4th generation composite bone, Sawbone, Sawbones Europe AB Malmo Sweden). This validated bone model has been previously used for several biomechanical studies, and its mechanical properties are similar to the tibia of a healthy adult without osteporosis13,14.
Six commercially available tibial intramedullary nails were used. They were all nine mm in diameter, with lengths ranging from 335 to 360 mm. The nails were composed of stainless steel or titanium alloy, were solid or cannulated, and they had various configurations of proximal and distal locking options. The distal holes ranged from two to four, and the proximal ones from two to five. The orientation of the proximal screws also varied, from the classic mediolateral to a combination of mediolateral, oblique, and anteroposterior (Table 1). The experiments took place between 2014 and 2017 at the laboratories of the Mechanical Engineering Department, School of Engineering, International Hellenic University, Serres, Greece. Implementation of this experimental study was approved by the General Assembly of the School of Medicine of the Aristotle University of Thessaloniki. Ethical approval was not required since there are no humans or animals involved in the experiments only model and material testing.
Specimen preparation
The sawbones were divided into six groups of five, and each group was prepared with one of the six nails. The bone model was stabilized using a custom-made clamp, and an identical entry point was established in all models based on similar landmarks on the tibial plateau. The medullary canal was entered using either an owl or a drill bit, depending on the surgical technique suggested by the manufacturer, followed by a guidewire. The canal of all the bone models was reamed up to 10.5 mm in 0.5 increments, and the nail was inserted until the proximal end of the implant stayed flush to the surface of the sawbone. Each nail was locked proximally with the maximum number of screws it allowed. Distally, all nails were locked with two screws, which were inserted either with the jig provided by the manufacturer or with a freehand technique under image intensification15. At this point, all specimens were radiographed with an anteroposterior and lateral view.
All specimens were marked at a distance of eight and ten cm below the articular surface of the tibial plateau. A two cm osteotomy was performed, using a handsaw. This osteotomy represents the worst-case scenario in terms of stability, simulating a 42-C3 fracture, according to the AO classification of long bones fractures, as in the technique used by Horn et al and Agathangelidis et al4,16-18.
Mechanical testing
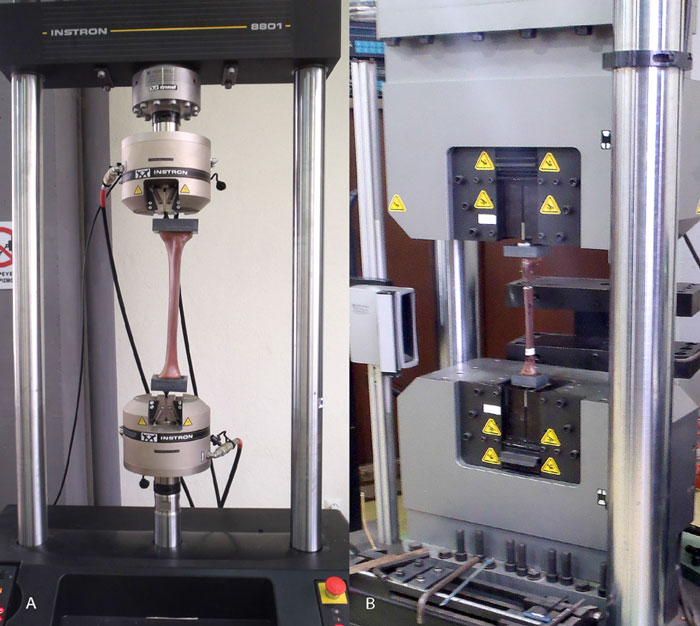
All specimens underwent biomechanical loading in two modes. The first mode was fatigue testing with low, eccentric loads for 100,000 cycles, and the second mode was axial static loading with higher loads (Figure 1).
Figure 1: Experimental setup for A) fatigue testing and B) static loading of the composite tibia models implanted with six different intramedullary nails.
For the first part of the experiment, the proximal and distal ends of the specimens were potted in a hollow-formed polyamide fixture, filled with fiberglass-reinforced resin. The molds did not encapsulate any screws and ensured that the load was shared evenly on the tibial plateau and plafond surfaces. The custom-made fixtures were marked at a point 23 mm medially to the anatomic axis of the tibia proximally and 9 mm medially to the same axis distally. This offset reproduces the expected peak load vector during the gait cycle19,20. The specimens were compressive cyclic loaded on the fatigue testing machine (Instron 8801, Instron, Pfungstadt, Germany) for 100,000 cycles. All the fatigue tests were conducted in load-controlled mode with a haversine loading of 2 Hz frequency. The dynamic loading, ranging from 200 N to 450 N, was imposed upon a static preload of 150 N in order to ensure that the specimen’s flexure would not lead to contact relaxation between the specimen and the fixture. The loading forces represent partial weight-bearing for a subject weighing 65 to 85 kg and were adapted from previous studies21. During the implementation of the fatigue tests in every 10.000 cycles, simultaneous load and displacement data acquisition were carried out. The quantitative outcome of all tests was the calculated value of dynamic stiffness, representing the specimen’s rigidity. The loading and data acquisition protocol was used before by Goett et al22. For the second part of the experiment, the specimens mounted on the custom-made fixtures were loaded on the compression testing machine (Instron Satec 1200, Instron, Pfungstadt, Germany), this time with the load passing along the anatomic axis of the tibia. The specimens were statically loaded for three cycles, with forces ranging from 100 N to 1200 N. In order to calculate each specimen’s stiffness, data acquisition was performed during the fourth cycle.
Statistical analysis
Descriptive statistics are reported as means ± standard deviation. Normality assumptions were evaluated using the Shapiro-Wilk test. One-way ANOVA was used for the comparison of means of independent measurements, while Generalized Estimating Equations (GEE) modeling was used for the assessment of the effects of independent factors/covariates on longitudinal measurements. The Sidak correction was used to adjust for multiple testing. Data analysis was performed with Stata 13.1 (Stata Corp., College Station, TX).
Results
Fatigue testing
During the first mode of the experiment, data acquisition was performed every 10,000 cycles while the stiffness of the construct was also calculated. For each specimen, a comparison of the stiffness of every step up to 100,000 cycles was performed in order to identify any irregular behavior or mechanical failure of the construct. Each specimen’s mechanical properties remained stable up to 100,000 cycles without any failure or irregularity.
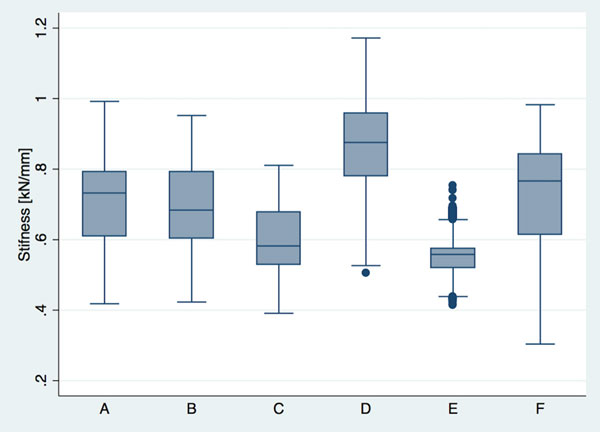
The average stiffness for each group was compared pairwise in a post hoc fashion (Table 2). Statistically significant differences between groups were detected at the 5 % level (F =36.8, df =5.19, p <0.001). Results of the post hoc procedure suggest that groups D and E differ from all others, with D having the highest values and E the lowest. The average stiffnesses of Groups F and B are very close; the same holds for groups A, B, and C. These results are illustrated in Figure 2.
Figure 2: Box plots comparing the stiffness of each group (of tibia models implanted with nails from different manufacturer) during fatigue testing.
Static loading
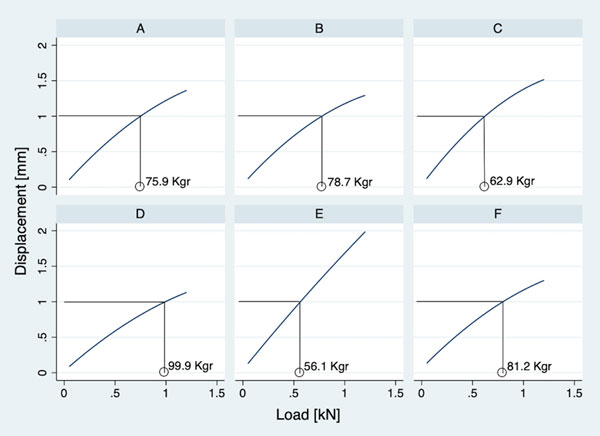
The average stiffness for each group was recorded in a longitudinal setting. Generalized Estimating Equations (GEE) modeling was used for inference as a result. Group D differs from all other models in this setting (p <0.05), giving the highest values, while group E differs from F only (p =0.024). In all other comparisons, there were no statistically significant differences (p >0.05) (Table 3; Figure 3).
Figure 3: Box plots comparing the stiffness of each group (of tibia models implanted with nails from different manufacturer) during static loading.
For each group of specimens, we additionally calculated the force needed to reach the limit of one mm of displacement at the fracture site. Group D recorded the highest value. A, B, and C did not differ significantly amongst them, E was similar to C but had significantly lower value both from A and B. Finally, group F had similar values to A and B but differed from all others (Figure 4).
Figure 4: The value of load causing displacement of one millimeter at the fracture site for each of the six groups (of tibia models implanted with nails from different manufacturers).
Footnote for figures 2-4
Group A: Dynamic T, Citieffe, (Bologna, Italy), Group B: Targon T, B-Braun Aesculap, (Tuttlingen, Germany), Group C: OrthoSelect Interlocking Nail system, (Wurmlingen, Germany), Group D: Orthofix Tibial nailing system, (Verona, Italy), Group E: T2, Tibial nailing system, Stryker, (Schönkirchen, Germany), Group F: Expert Tibial Nail, Depuy Synthes (Oberdorf,Switzerland).
Discussion
In the present study, we experimented with the biomechanical behavior of six different intramedullary nails. Solid stainless steel nails, with two oblique screws and cannulated titanium nails with five proximal screws, outperformed all other nails in terms of stability. The nails were implanted in composite tibia bone models, which have been widely used in biomechanical studies23. Their mechanical properties are consistent and predictable compared to cadaveric tibiae; they are available in large numbers and assure uniformity. As a result, any differences we found between the various specimens were attributed to the mechanical properties of the nail and not to the bone model. We also used a wide osteotomy of the proximal metaphysis like the one used by Hansen et al and Laflamme et al, simulating the worst-case scenario of an extra-articular fracture of the proximal tibia in terms of stability, since there is no cortical contact of the fracture fragments, no soft tissue stabilization and the stability of the fracture depends solely on the implant12,16. During fatigue testing, we loaded the bone models in an axis medial to the anatomic axis of the tibia. This loading mode, that was proposed by Gaebler et al and has been implemented in a number of studies, simulates the location of the expected resultant load during peak loading19,20. During static loading, we used the anatomic axis of the model to apply higher but non-destructive forces. Regarding stiffness, the results were similar in these two testing modes in terms of grouping: in both tests, group D had the highest stiffness values, while group E had the lowest ones. However, in the eccentric loading, the differences observed between the various models were more distinct.
There are various studies in the literature which are focused on a proximal tibial fracture and its optimal treatment. In a cadaveric study, Feng et al compared a nail with two proximal screws with plating and external fixation systems24. They found that the nail had adequate mechanical properties in compression but not in bending. The authors concluded that a titanium nail with two screws is not adequately stable and should be assisted with a plate. In our study, we found that titanium nails with more than three screws outperformed titanium nails with only two or three screws. Therefore, more proximal locking options could render the need for adjuvant methods of fixation unnecessary.
Laflamme et al compared a tubular tibial nail to a plate. The authors concluded that in terms of stability, a construct with a nail and four proximal screws was similar to a plate osteosynthesis12. They also found that the removal of the two oblique screws, in all testing modes, significantly decreased the rigidity of the system. Three out of the six nails we tested were tubular, titanium with a range of three to five screws. We found that group E that had the maximum number of proximal screws in various directions was stiffer, followed by group A that had three screws, two lateral and one anteroposterior, and then by group E that had two oblique and one dynamic lateral. Our results agree with Laflamme’s, in that more screws in more than one direction add to the stability of the nail construct.
In a biomechanical test, Gollwitzer et al, found that two proximal screws were more stable than one; when they used only one screw, the construct was stiffer only when they increased the distance of the screws from the knee joint25. We did not test any nails with less than two locking options, but we found that the second-best group in terms of stability was with that with the maximum number of screws and the most distal screw closest to the fracture, compared to all other nails. However, the stablest construct had only two oblique screws and was relatively close to the knee joint. This shows that other mechanical factors play a more critical role than the distance from the knee joint.
In a biomechanical study, Weninger et al compared solid and cannulated tibial nails for the treatment of unstable distal tibial fractures. The authors concluded that screw failures occurred earlier with cannulated nails than with solid ones26. To the best of our knowledge, this is the only study that directly compares these two types of nails and shows that screw number and configuration are very important in cannulated nails, since the load shared from the nail to the locking configuration may lead to mechanical failure. In line with the interpretation given by Weninger et al, our data suggest that a solid nail with only two oblique screws (group D) is stiffer than a cannulated one with five screws (group E), in both static and dynamic loading.
There are a few papers in the literature supporting the use of the maximum number of screws for the intramedullary nailing of proximal tibial fractures. Hansen proved that three screws provide significantly more stability compared to two. Freeman showed that four screws perform better than three, while Kandemir concluded that a nail with four proximal screws provides similar fatigue performance to double locking plates16,19,27. Of the three cannulated nails in our experiment, the stablest of all was the one with five screws (group F), while the least stable of all was the nail with three screws, two oblique and one lateral (group E). Group A that had two lateral and one anteroposterior showed better mechanical stability than group E, which we attributed to the locking pattern in multiple directions.
It has been suggested that controlled micro-motion at a range of 0.2 to 1 mm at the fracture site will promote healing28. However, a system that is too stiff or very flexible will lead to delayed union, non-union, and eventually implant failure, if left untreated. In our results of static loading, we used a cut-off point of one mm of displacement and compared the forces required to reach that point. We came to the conclusion that on this mechanical model, a person weighing up to 100 kg can fully weight bear with a nail from group D without creating excessive motion at the fracture site that is more than one mm. On the other hand, nails from group E allow excessive micro-motion, when a person weighs more than 56.1 kg when the person fully weight bears. As a result, with regard to postoperative instructions, it is mandatory to take into account the patient’s weight: Until there are signs of fracture healing, patients are advised to partially weight bear with a load generally less than 50 kg.
To the best of our knowledge, the present study is the first to compare six different commercially available intramedullary nails for the treatment of unstable proximal tibial fractures. Every effort was made to exclude other mechanical factors and compare only the behavior of the implants in terms of stability, which is of the utmost importance when it comes to fracture healing. Limitations of our study include the relatively small number of specimens and testing in only two loading modes.
In the past, intramedullary nailing has been considered an unsafe method for the treatment of proximal tibial fractures. We believe that with the flexibility of proximal screw configuration that recently developed implants offer, intramedullary nailing has become a safe and reasonable option for these fractures.
The present study showed that the solid stainless steel nail from Orthofix (Verona, Italy) with two oblique proximal screws was better in terms of mechanical stability, followed by the Expert cannulated titanium nail from Depuy-Synthes (Oberdorf, Switzerland) with five proximal screws.
Conflict of interest
The authors declare that there is no conflict of interest and they have no proprietary interests in the materials described in the article.
References
1. Alho A, Benterud JG, Høgevold HE, Ekeland A, Strømsøe K. Comparison of functional bracing and locked intramedullary nailing in the treatment of displaced tibial shaft fractures. Clin Orthop Relat Res. 1992: 243-250.
2. Schmidt AH, Finkemeier CG, Tornetta P 3rd. Treatment of closed tibial fractures. Instr Course Lect. 2003; 52: 607-622.
3. Freedman EL, Johnson EE. Radiographic analysis of tibial fracture malalignment following intramedullary nailing. Clin Orthop Relat Res. 1995: 25-33.
4. Agathangelidis F, Petsatodis G, Kirkos J, Papadopoulos P, Karataglis D, Christodoulou A. Distal Locking Screws for Intramedullary Nailing of Tibial Fractures. Orthopedics. 2016; 39: e253-e258.
5. Mohammed A, Saravanan R, Zammit J, King R. Intramedullary tibial nailing in distal third tibial fractures: distal locking screws and fracture non-union. Int Orthop. 2008; 32: 547-549.
6. Lang GJ, Cohen BE, Bosse MJ, Kellam JF. Proximal third tibial shaft fractures. Should they be nailed? Clin Orthop Relat Res. 1995: 64-74.
7. Wolinsky PR, Dennis D, Crist BD, Curtiss S, Hazelwood SJ. The biomechanics of varied proximal locking screw configurations in a synthetic model of proximal third tibial fracture fixation. J Orthop Trauma. 2011; 25: 175-179.
8. Krettek C, Stephan C, Schandelmaier P, Richter M, Pape HC, Miclau T. The use of Poller screws as blocking screws in stabilising tibial fractures treated with small diameter intramedullary nails. J Bone Joint Surg Br. 1999; 81: 963-968.
9. Buehler KC, Green J, Woll TS, Duwelius PJ. A technique for intramedullary nailing of proximal third tibia fractures. J Orthop Trauma. 1997; 11: 218-223.
10. Tornetta P 3rd, Collins E. Semiextended position of intramedullary nailing of the proximal tibia. Clin Orthop Relat Res. 1996: 185-189.
11. Franke J, Hohendorff B, Alt V, Thormann U, Schnettler R. Suprapatellar nailing of tibial fractures-Indications and technique. Injury. 2016; 47: 495-501.
12. Laflamme GY, Heimlich D, Stephen D, Kreder HJ, Whyne CM. Proximal tibial fracture stability with intramedullary nail fixation using oblique interlocking screws. J Orthop Trauma. 2003; 17: 496-502.
13. Lasanianos NG, Garnavos C, Magnisalis E, Kourkoulis S, Babis GC. A comparative biomechanical study for complex tibial plateau fractures: nailing and compression bolts versus modern and traditional plating. Injury. 2013; 44: 1333-1339.
14. Schuller M, Weninger P, Tschegg E, Jamek M, Redl H, Stanzl-Tschegg S. Micromotion at the fracture site after tibial nailing with four unreamed small-diameter nails–a biomechanical study using a distal tibia fracture model. J Trauma. 2009; 66: 1391-1397.
15. Whatling GM, Nokes LD. Literature review of current techniques for the insertion of distal screws into intramedullary locking nails. Injury. 2006; 37: 109-119.
16. Hansen M, Mehler D, Hessmann MH, Blum J, Rommens PM. Intramedullary stabilization of extraarticular proximal tibial fractures: a biomechanical comparison of intramedullary and extramedullary implants including a new proximal tibia nail (PTN). J Orthop Trauma. 2007; 21: 701-709.
17. Horn J, Linke B, Höntzsch D, Gueorguiev B, Schwieger K. Angle stable interlocking screws improve construct stability of intramedullary nailing of distal tibia fractures: a biomechanical study. Injury. 2009; 40: 767-771.
18. Rüedi TP, Murphy WM. AO principles of fracture management. 2nd Edition. AO Pub., Switzerland; Theme, Stuttgart, New York, 2007.
19. Freeman AL, Craig MR, Schmidt AH. Biomechanical comparison of tibial nail stability in a proximal third fracture: do screw quantity and locked, interlocking screws make a difference? J Orthop Trauma. 2011; 25: 333-339.
20. Gaebler C, Speitling A, Milne EL, Stanzl-Tschegg S, Vecsei V, Latta LL. A new modular testing system for biomechanical evaluation of tibial intramedullary fixation devices. Injury. 2001; 32: 708-712.
21. Gueorguiev B, Wähnert D, Albrecht D, Ockert B, Windolf M, Schwieger K. Effect on dynamic mechanical stability and interfragmentary movement of angle-stable locking of intramedullary nails in unstable distal tibia fractures: a biomechanical study. J Trauma. 2011; 70: 358-365.
22. Goett SD, Sinnott MT, Ting D, Basinger RR, Haut RC, Dejardin LM. Mechanical comparison of an interlocking nail locked with conventional bolts to extended bolts connected with a type-IA external skeletal fixator in a tibial fracture model. Vet Surg. 2007; 36: 279-286.
23. Burton NJ, Fitzpatrick N, Wallace AM. Evaluation of cut accuracy and cis cortical damage for tibial plateau leveling osteotomy performed with and without aid of a novel saw guide: an in vitro study. Vet Surg. 2013; 42: 28-37.
24. Feng W, Fu L, Liu J, Qi X, Li D, Yang C. Biomechanical evaluation of various fixation methods for proximal extra-articular tibial fractures. J Surg Res. 2012; 178: 722-727.
25. Gollwitzer H, Karampour K, Hauschild M, Diehl P, Busch R, Mittelmeier W. Biomechanical investigation of the primary stability of intramedullary compression nails in the proximal tibia: experimental study using interlocking screws in cryopreserved human tibias. J Orthop Sci. 2004; 9: 22-28.
26. Weninger P, Schueller M, Jamek M, Stanzl-Tschegg S, Redl H, Tschegg EK. Factors influencing interlocking screw failure in unreamed small diameter nails–a biomechanical study using a distal tibia fracture model. Clin Biomech (Bristol, Avon). 2009; 24: 379-384.
27. Kandemir U, Herfat S, Herzog M, Viscogliosi P, Pekmezci M. Fatigue Failure in Extra-Articular Proximal Tibia Fractures: Locking Intramedullary Nail Versus Double Locking Plates-A Biomechanical Study. J Orthop Trauma. 2017; 31: e49-e54.
28. Claes LE, Heigele CA, Neidlinger-Wilke C, Kaspar D, Seidl W, Margevicius KJ, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop Relat Res. 1998: S132-S147.