CASE REPORT
Hippokratia 2016, 20(3):235-237
Kamperidis V1, Michou E1, Kouskouras K2, Nikolaidou O2, Karvounis H1
11st Cardiology Department, 2Radiology Department, AHEPA Hospital, Medical Faculty, Aristotle University of Thessaloniki, Thessaloniki, Greece
Abstract
Background: Contrast-enhanced transesophageal echocardiography (TEE) for the opacification of left atrial appendage (LAA) is not clearly suggested by the current guidelines and only scarce data are available.
Case Presentation: A patient with a membrane-like structure in the LAA cavity is presented. Contrast-enhanced TEE revealed LAA pericardial effusion and this diagnosis was confirmed by cardiac magnetic resonance that offered comparable images and tissue characterization.
Conclusion: Contrast-enhanced TEE has been demonstrated to safely and accurately enlighten LAA anatomy. Hippokratia 2016, 20(3): 235-237
Key words: Left atrial appendage, contrast-enhanced echocardiography, transesophageal echocardiography, cardiac magnetic resonance, pericardial fluid
Corresponding author: Vasileios Kamperidis MD, MSc, PhD, FESC, 1st Cardiology Department, AHEPA University Hospital, 1 St.Kyriakidi str., 54636, Thessaloniki, Greece, tel: +302310994830, fax: +302310994830, e-mail: vkamperidis@outlook.com
Introduction
The presence of pericardial effusion in the area of left atrial appendage (LAA) although rare and benign may sometimes be mistaken for other pathologies, such as obstructive and non-obstructive membranes1, intra-atrial masses and thrombi2. Transesophageal echocardiography (TEE) is a safe and readily accessible imaging modality used for LAA assessment. Its advantages over other imaging modalities include portability, best spatial (0.2-0.5 mm) and temporal (20-33 msec) resolution, and lack of nephrotoxicity and ionizing radiation3. However, scarce data exist for contrast-enhanced TEE for differentiating between LAA pathologies.
We report the case of a patient in whom differential diagnosis of a membrane-like structure in the LAA was made successfully and accurately by contrast-enhanced TEE. Cardiac magnetic resonance (CMR) confirmed the TEE diagnosis.
Case presentation
A 54-year-old man with fever of unknown origin over the preceding three months was investigated for endocarditis. The patient was a previously healthy man and the physical examination was unremarkable. The electrocardiogram showed normal sinus rhythm. Transthoracic echocardiography demonstrated normal left ventricular size, wall thickness and systolic function, no evidence of vegetations and a trivial circumferential pericardial effusion. Although TEE revealed no vegetation, a thin and mobile membrane-like structure was demonstrated in the LAA, looking like dividing it into two chambers (Figure 1A). In order to better visualize the LAA, echo contrast was administered. After echo contrast injection, the LAA was opacified leaving an echolucent space around it, consistent with pericardial effusion in the transverse sinus of the pericardium whereas no thrombi or intracardiac membrane were documented (Figure 1B). CMR (supplementary video 1) confirmed the diagnosis of small pericardial effusion around the LAA (Figure 1C), matching with contrast-enhanced TEE images (Figure 2).
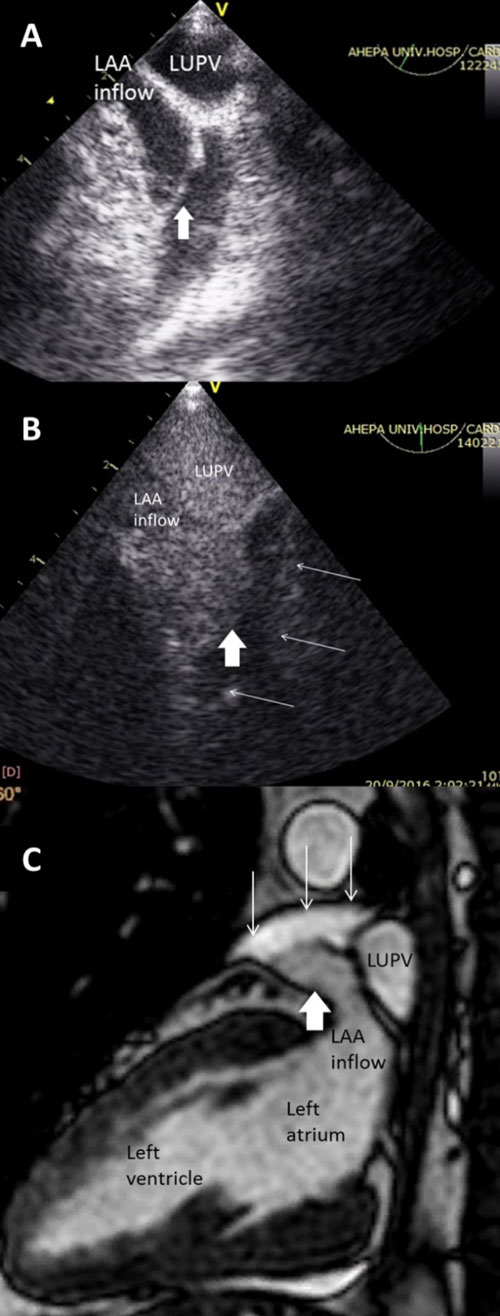
Figure 1: A) Transesophageal echocardiography (TEE) zoomed view of the left atrial appendage (LAA) at 60o showing the presence of a membrane-like structure within the LAA (white arrow). B) Contrast-enhanced TEE zoomed view of the LAA showing complete opacification of the LAA (thick white arrow), differentiating it from the surrounding pericardial fluid (multiple thin white arrows). C) Cardiac magnetic resonance long axis view delineating the LAA and differentiating it by tissue characterization from the surrounding pericardial fluid.
LAA: left atrial appendage, LUPV: left upper pulmonary vein.

Figure 2: The contrast-enhanced transesophageal echocardiography view of the left atrial appendage (A) is comparable to the cardiac magnetic resonance image of it (B). In both images, the thick white arrow points the left atrial appendage and the multiple thin white arrows the surrounding pericardial fluid.
LUPV: left upper pulmonary vein.
Discussion
The current case suggests that contrast-enhanced TEE safely elucidates LAA pathology and accurately identifies the presence of pericardial effusion in the transverse sinus, around LAA.
The LAA is a remnant of the embryonic left atrium, lying in the left atrioventricular groove where it is in close relation with the left circumflex artery, the left superior pulmonary vein posteriorly and the mitral valve annulus medially4. It is a finger-like projection of the left atrium that varies markedly in shape, volume, length, width and orifice size and shape. The LAA lies within confines of the pericardium and is closely related to the pulmonary artery in its superior aspect and to the free wall of the left ventricle inferiorly5. The transverse sinus is an extension of the pericardium between the ascending aorta and the left atrium. It is visualized only when fluid is present, and in such a condition the wall of the LAA may appear as a mobile mass inside this fluid-filled space mimicking a mass lesion or a membrane-like structure5. In the current case, this picture of LAA as a pseudomass was accurately visualized by contrast-enhanced TEE and CMR.
TEE is currently the most widely used imaging modality for the assessment of LAA morphology, size, and the presence of spontaneous echo contrast or thrombi. It is indicated in patients with new-onset atrial fibrillation before rapid cardioversion and ablation of elective atrial arrhythmia, particularly when the patient is not anticoagulated properly or is at high risk for stroke6. Moreover, TEE guides the implantation of LAA closure devices, ensuring a complication-free and successful procedure7. Although TEE offers a good and safe visualization of LAA, imaging artifacts and lack of tissue characterization challenge the determination of its margins. In such cases, the use of ultrasound contrast agents may be considered. However, scarce evidence exists on the use of contrast; The European guidelines do not refer to it, and the American guidelines suggest it as a new future modality8,9. Only a limited number of cases report its use for better visualization of LAA; Bernier et al10 and Jung et al11demonstrated that in patients with atrial fibrillation, contrast enhanced TEE performed prior to cardioversion, detects LAA thrombi accurately and diminishes embolic events. The current case demonstrated that contrast opacified LAA and differentiated it from the surrounding pericardial fluid in transverse sinus, while the membrane-like structure in LAA before the contrast use, proved to be the LAA’s thin wall suppressed by the pericardial effusion.
CMR was used to double-check and differentiate between LAA membrane and pericardial fluid. CMR is an emerging modality for imaging cardiac structure/function and tissue characterization. It has been suggested that it may be equally effective as TEE in detecting thrombus in LAA12. However, it has drawbacks that limit its use: lowest spatial resolution, prolonged examination duration, higher cost, dependence on breath hold, and inability to be performed in patients with implanted cardiac devices and real-time during procedures3. In the current case, CMR confirmed the contrast-enhanced TEE diagnosis by providing comparable images (Figure 2) and by tissue characterization (Figure 3) confirmed that the non-enhanced on contrast-echocardiography structure around LAA was pericardial fluid.
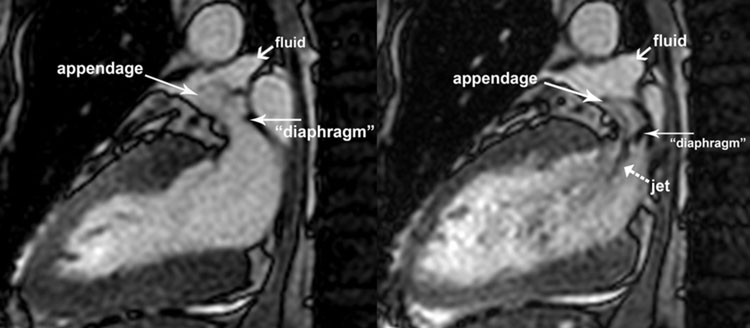
Figure 3: The cardiac magnetic resonance imaging in systole and diastole identifies the cardiac structures around the left atrial appendage, as indicated by the arrows, and provides tissue characterization.
Conclusion
Contrast-enhanced TEE has been demonstrated to safely and accurately enlighten LAA anatomy. It revealed the presence of pericardial fluid surrounding LAA and excluded the presence of membrane and thrombi, sparing unnecessary medication and additional costly, nephrotoxic and time-consuming investigations for the patient.
Conflict of interest
None declared by authors.
Acknowledgement
In the electronic version of the paper Supplementary Video 1 shows CMR sine view.
References
1. Bakris N, Tighe DA, Rousou JA, Hiser WL, Flack JE 3rd, Engelman RM. Nonobstructive membranes of the left atrial appendage cavity: report of three cases. J Am Soc Echocardiogr. 2002; 15: 267-270.
2. Messas E, Szymanski C, Fabiani JN, Desnos M, Hagege A. Pericardial effusion causing echocardiographic mimicking of left intra-atrial thrombus. Eur J Echocardiogr. 2009; 10: 353-355.
3. Beigel R, Wunderlich NC, Ho SY, Arsanjani R, Siegel RJ. The left atrial appendage: anatomy, function, and noninvasive evaluation. JACC Cardiovasc Imaging. 2014; 7: 1251-1265.
4. Regazzoli D, Ancona F, Trevisi N, Guarracini F, Radinovic A, Oppizzi M, et al. Left Atrial Appendage: Physiology, Pathology, and Role as a Therapeutic Target. Biomed Res Int. 2015; 2015: 205013.
5. Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999; 82: 547-554.
6. Grewal GK, Klosterman TB, Shrestha K, Yarmohammadi H, Zurick AO, Varr BC, et al. Indications for TEE before cardioversion for atrial fibrillation: implications for appropriateness criteria. JACC Cardiovasc Imaging. 2012; 5: 641-648.
7. Palios J, Paraskevaidis I. Thromboembolism Prevention via Transcatheter Left Atrial Appendage Closure with Transeosophageal Echocardiography Guidance. Thrombosis. 2014; 2014: 832752.
8. Senior R, Becher H, Monaghan M, Agati L, Zamorano J, Vanoverschelde JL, et al. Contrast echocardiography: evidence-based recommendations by European Association of Echocardiography. Eur J Echocardiogr. 2009; 10: 194-212.
9. Porter TR, Abdelmoneim S, Belcik JT, McCulloch ML, Mulvagh SL, Olson JJ, et al. Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiogr. 2014; 27: 797-810.
10. Bernier M, Abdelmoneim SS, Stuart Moir W, Eifert Rain SS, Chandrasekaran K, Ammash NM, et al. CUTE-CV: a prospective study of enhanced left atrial appendage visualization with microbubble contrast agent use during transesophageal echocardiography guided cardioversion. Echocardiography. 2013; 30: 1091-1097.
11. Jung PH, Mueller M, Schuhmann C, Eickhoff M, Schneider P, Seemueller G, et al. Contrast enhanced transesophageal echocardiography in patients with atrial fibrillation referred to electrical cardioversion improves atrial thrombus detection and may reduce associated thromboembolic events. Cardiovasc Ultrasound. 2013; 11: 1.
12. Rathi VK, Reddy ST, Anreddy S, Belden W, Yamrozik JA, Williams RB, et al. Contrast-enhanced CMR is equally effective as TEE in the evaluation of left atrial appendage thrombus in patients with atrial fibrillation undergoing pulmonary vein isolation procedure. Heart Rhythm. 2013; 10: 1021-1027.
